Health Management
Bloat
Causes
- Lush, young pastures and leaves containing high concentration of soluble protein and dominated legume plants particularly alfalfa, red and white clovers and occurs with grazing of young green cereal crops, rape, turnips and legume vegetable crops.
- Feeding of high quality hay.
- Feeding of high grain diet.
- Feeding of the finely ground feed.
- Physical obstruction to eructation occurs in esophageal obstruction caused by a foreign body, pressure outside the esophagus and obstruction of cardia.
Clinical symptoms
- Obvious distention of the rumen and entire abdomen.
- Discomfort with the animal may stand and lying down frequently, kicking at its abdomen and rolling.
- Sudden death with distended abdomen.
- Dyspnea and grunting accompanied by mouth breathing
- Protrusion of the tongue and extension of the head.
Suggested first aid
- The passage of a stomach tube or trocarization to release large quantities of gas.
- An incision of about 10-20 cm in length over the left paralumbar fossa through the skin, abdominal musculature and directly into the rumen.
- A stick is tied in the mouth like a bit to promote the production of excessive saliva.
- Administration of antifoaming agents such as vegetable oils (peanut, corn, soybean) and mineral oils (paraffin) at doses of 80-250 ml.
Control and prevention
- The pasture should be free from leguminous fodders and bloat producing plants.
- Feeding hay before turning cattle on pasture.
- Maintaining grass dominance in the sward or using strip grazing to restrict intake.
- Allowing animals on well grown mature pastures than immature or rapidly growing pastures.
- Grass- legume mixture with a legume content of 50% is suggested as the maximum bloat safe level.
- Prevention of high energy and high protein supplement.
- Drenching of 60-120 ml of antifoaming agents twice daily (at milking times).
- Feedlot rations should contain at least 10-15% cut or chopped roughage mixed into the complete feed. Preferably the roughage should be a cereal, grain straw, grass hay.
- Grains should be rolled or cracked, not finely ground.
- Pelleted rations made from finely ground grain should be avoided.
Enteritis
Causes
- The enteropathogens like bacteria, viruses, fungi, protozoa and helminths, chemical and toxins.
Clinical symptoms
- Diarrhea
- Dehydration, abdominal pain, septicemia and toxemia with fever.
- Feces are soft or fluid in consistency and unpleasant odor.
- Contain blood, mucus/ foreign materials like sand.
- Color of feces is pale yellow and sometimes frank blood.
- Distribution of the feces on animal’s perineum.
Control
- Reduce infection pressure
- Ensure adequate non specific resistance by adequate colostrum intake
- Vaccinate for those diseases for which there is an effective vaccine
- Minimize Managemental and environmental stressors.
Thelitis
- This condition is inflammation of teat due to entry of pathogens into teat.
- It most commonly occurs in milch animals.
- It is due to unhygienic measures and environment.
- This causes no change in colour and consistency of milk.
- Untreated teat results in complete destruction of teat.
Clinical symptoms
- Affected teat initially shows reddening and swelling of teat.
- Infection progress leads to inflammation of teat.
- Decreased milk production.
- Severe infection leads to destruction of affected teat.
Prevention and control
- The animal’s environment should be clean and hygienic.
- The floor of the milch animal should be periodically cleaned with antiseptic solution.
- The milker’s hand should be clean before each milking.
- The dipping of teat after each milking may be effective in preventing entry of pathogens into teat.
- Affected animals should be given with earlier treatment to avoid destruction of teat.
- Affected animal’s teat should be treated with qualified veterinary doctor.
Abortion
- This is expulsion of dead or live recognizable size fetus prior to expected date of calving and this may be due to various causes.
Causes
- Infectious conditions such as Bovine Viral Diarrhea (BVD), Infectious Bovine Rhinotracheitis (IBRT), Leptospirosis, Brucellosis, Mycotic abortion, Actinomyces, Trichomoniasis, Campylobacteriosis, Listeriosis, Chlamydiosis, and Epizootic Bovine Abortion may cause abortion in cattle.
- Severe trauma, severe torsion of the uterus and twinning may cause abortion.
- Toxins can cause abortion in cows.
- Coumarins from rat poison and moldy sweet clover can cause abortion.
- Nitrates, chlorinated napthalenes, arsenics can cause abortion.
- Locoweeds, perennial broom weed and pine needles can cause abortion.
- Estrogenic compounds may cause abortion.
- Douching and infusion or Artificial insemination of the pregnant animals causes abortion.
- Vitamin A, iodine and selenium deficiencies can cause abortion.
Clinical signs
- Expulsion of water bag or severe mucus discharges from vulva in gestation period.
- Anorexia, dull and depressed condition of animal.
- Spontaneous expulsion of recognizable size fetus.
Prevention and control measures
- Proper disposal of the aborted fetus and its membranes.
- Prevention of contamination from infected materials (uterine discharges, fetal membranes)
- Always the animal shed should be clean.
- For Infectious Bovine Rhinotracheitis and Infectious Pustular Vulvovaginitis (IBR-IPV) pregnant cows at any stage of gestation should not be vaccinated with IBR-IPV vaccine. Vaccination can be carried out in heifers at 6-8 months of age.
- To prevent abortion due to listeriosis, feeding of poor quality silage with high pH should be prevented.
- To prevent abortion due to brucellosis, vaccination of calves from 3 to 7 months of age with strain 19 brucella vaccine and bull calves should not be vaccinated.
- Breeding should be stopped during disease outbreak.
- Contact between animals should be kept at a minimum during outbreak.
- Diseased bulls should not be used for breeding.
- The semen which is used for Artificial Insemination should be free from any infectious agents.
- Pregnant animals should be protected from other animals attack.
- Pregnant animal sheds should not be slippery.
Foot and Mouth Disease
About this disease
- This is a highly infectious viral disease of farm animals.
- This disease mostly manifests the lesions in the mouth, feet and mammary gland.
- Milk yield drops dramatically in milking animals, suckling calf usually die and pregnant animals may abort and infertility may ensure following abortion.
Causes
- It is caused by a virus Apthous of the family Picornaviridae.
Mode of Transmission
- Generally by direct or indirect contacts between susceptible and infected animals.
- Through movement of clinically affected animals.
- Through inanimate vectors such as vehicles, fodders, utensils, equipments etc.,
- Through air. Infected animals have a large amount of aerosol virus in their exhaled air, which can infect other animals via the respiratory or oral routes. The virus can travel up to 60 km overland and 300 km by sea.
- All secretions and excretions from the infected animal such as saliva, faeces and urine. The virus may be present in milk and semen for up to 4 days before clinical signs appear.
- The disease has been transmitted to calves via infected milk.
- This virus can survive in dry fecal material for 14 days in summer, in slurry up to 6 months in winter, in urine for 39 days and on the soil between 3 (summer) and 28 days (winter).
- By consumption of infected meat and meat by-products, unprocessed and uncooked milk.
- Through animal handlers, visitors and physicians.
- Most of the animals remain as a carrier following recovery after infection. Carrier may transfer the virus from one animal to another. Carrier cattle may harbor the virus in the esophageal-pharyngeal fluid for 6-24 months.
Symptoms
- High fever up to 104-106˙F (41˙C) and anorexia.
- Profuse salivation (saliva hanging in long ropy strings up to the ground).
- Animal stamps its feet and wounds in the inter-digital space of legs followed by lameness.
- Oral ulcers and lesions.
- Smacking of lips.
- Vesicles in the mammary gland.
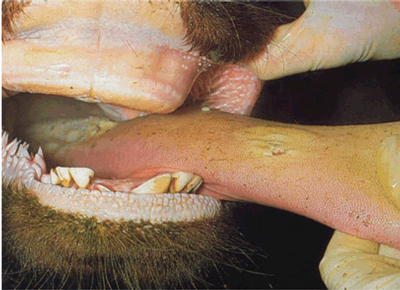
Disease Symptoms in the Mouth


Disease Symptoms in the Foot


Preventive measures
- We should provide most comfortable bedding prior to calving and in advanced stage of pregnancy. Sand is the ideal bedding material.
- Early detection and treatment of milk fever.
- Recently calved animals should be monitored at least 48 hours after parturition for the occurrence of milk fever signs.
- Recumbent animals should be treated as soon as possible and not delayed for more than 1 hour.
- Cow should not be mated with a heavy bull. The weight of the bull should be within the weight bearing capacity of the cow. Otherwise there is risk of paralysis and fracture of hip bones.
- The cow should be bred with a bull as per its size as a big calf in a small cow will invite dystocia problem leading to calving paralysis.
- Cow should not be made over fatty through too much feeding during advance pregnancy.
- Cow should be made to stand within a short time following parturition.
- Parenteral Vitamin D3 should be given in milk fever prone cow during pregnant period.
- Low calcium and high phosphorus diet should be given to stimulate parathyroid gland and thus to avoid hypocalcaemia.
- If possible cow of a dairy farm should be brought under metabolic profile test to pinpoint the deficit and to make good use of it.
Control measures
- Recumbent animals should be treated as soon as possible and not delayed for more than 1 hour.
- Provision of comfortable bedding materials for recumbent animals. Arrangement of soft bed should be made.
- Attempt should be made to roll the cow from side to side to minimize the extent of ischemic necrosis.
- Lift the cow and frequent turning should be made. Cow should be turned at least at 3 hours interval.
- Attempt should be made to lift the cow on its fore legs by using body slings.
- Hip lifters may be used for lift the downer animals.
- With the help of body slings, the animals should be allowed to stand for 20-30 minutes and then lowered down. This should be repeated several times a day.
- Animal’s both fore and hind limbs should be massaged two times per day.
- Downer animals should be milked normally and the udder kept clean by washing with germicide soap before milking and post milking teat dips should be applied.
- Re-placement therapy with Calcium, Phosphorus, magnesium, Glucose containing preparations can be used parentally by qualified veterinarian.
- Infective causes should be brought under antibiotic coverage.
- Physiotherapy by adopting muscle massage may be made to restore muscle activity of the limbs.
Retained Fetal Membranes (RFM)
Primary symptoms
- Hanging of fetal membranes from the vulva
About this condition
- This is one of the most common conditions occurring in animals following parturition.
- This is failure of the villi of the fetal cotyledon to detach from the maternal crypts of the caruncles and retained longer than normal time limits.
- If the placenta is retained longer than 8-12 hours the condition is considered as pathological.
Causes
- Infections of uterus during gestation may be a cause for retained placental membranes.
- Uterine inertia due to hormonal imbalance such as low level of oxytocin.
- Deficiency of Vitamin A and iodine causes retained placenta.
- The hormone progesterone and excess of cortisol in late gestation may cause the retention of fetal membranes.
- The disease conditions causing uterine inertia or atony results in a higher incidence of retention of foetal membranes.
- Close confinement and lack of exercise highly prone to retained placenta.
Clinical signs
- A portion of the fetal membranes hang from the vulva 12 hours or more even after the expulsion of the foetus.
- Anorexia and depression may develop.
- A fetid odour develops since the placenta begins to macerate after 24 hours of foetal expulsion.
Treatment
- It should be handled with qualified veterinary doctor by manual removal.
- Before arriving veterinarian, the hanging foetal membranes should be protect from dogs or other animals.
- The protruding membranes should be tied in a knot to prevent them touching the hocks.
- Manual removal can be attempted in 24- 48 hours after parturition.
- Manual removal after 48 hours is not advisable because cervix was closed.
- Manual removal of placenta is contraindicated in cows with elevated temperature and also with vaginitis and vulvitis.
- After removing the fetal membranes, tetanus toxoid injection is recommended to prevent tetanus infection.
Total uterine Prolapse
Primary symptom
- A mild protrusion of the vaginal mucous membrane through the vulval lips.
Secondary symptom
- The prolapsed mass hanging upto the hock joint.
About this condition
- This is expulsion of uterine mass through the vagina.
- It is a common complication of third stage of labour.
- It is more common in pluriparous than primiparous animals.
- This condition is most commonly seen in cow than other animals.
Causes
- The flaccid atonic uterus.
- Violent or strong tenesmus during or after parturition.
- Retention of placenta at the ovarian pole of the uterine horn.
- Excessive relaxation of the pelvic and perineal region.
- Commonly seen in confined or stabled cattle especially during winter months.
- Forced extraction of the fetus.
- Over distension of the abdomen or excessive amounts of loose pelvic fat favour the condition by increasing the intra-pelvic pressure.
- Due to intra abdominal pressure.
- Delayed contraction of the uterus.
- Poorly grown, thin debilitated heifers and low plan of nutrition.
- During last 2-3 months of gestation, when large amounts of oestrogenic hormone being secreted by the placenta known as hyper estrogenism.
Symptoms
- A mild protrusion of the vaginal mucous membrane through the vulval lips when the animal lies down.
- In standing posture, the prolapsed mass hanging upto the hock joint.
- The fetal membranes and /or mucus membrane of the uterus is exposed.
- The mass is usually covered with feces, straw, dirt or blood clots.
- Uterus is enlarged and edematous especially in delayed cases (4-6 hrs).
- The cervix is usually present at the vulva.
- The non gravid horn is held inside the peritoneal surfaces of the prolapsed gravid horn and does not evert.
- Stress, restlessness, pain, anxiety, increased respiratory rate may be noticed.
- Internal hemorrhage due to rupture of one of the uterine vessels, shock, incarceration of the intestinal mass and death.
- Pale mucus membrane, expiratory grunt and prostration with severe depression and inability to rise indicated serious complications.
Suggested first aid
- The prolapsed animal should be separated from other animals.
- The mass should be protected from contamination from out sources.
- The mass should be covered with wet clean clothes until treatment.
- It needs careful insertion of protruded uterine mass into the body and suturing the in the vulval lips so this condition should be handled with qualified veterinary doctor.
Source: Expert System for Cattle & Buffalo, Directorate of Extension Education, TANUVAS
Vaccination schedule for dairy cattle
| S.No | Age | Vaccine |
|---|---|---|
| 1 |
| Foot and mouth disease (FMD) vaccine- 1st dose FMD - Second dose FMD - Booster |
| 2 | Six months | Anthrax vaccine Black quarter (BQ) vaccine |
| 3 | After Six months | Haemorrhagic septicaemia (H.S) vaccine |
| 4 | Yearly Once | BQ, H.S and Anthrax |
Comments
Post a Comment